Samantha Destura
The Role of Nutrition in Cancer Care
Summary
This study aims to identify and understand the main challenges and barriers for nutritional support resource options according to hospital or outpatient center location (US & UK) and the cancer stage and type. The main form of data collection was qualitative through semi-structured interviews with oncologists, registered dietitians, clinical nurse specialists, research scientists, and patients. Findings informed the second phase, which generated a potential solution to help improve the situation regarding cancer-associated malnutrition and cachexia detection and management among patients.
Additional info
Research Questions
Main Question
- How might we further integrate Medical Nutrition Therapy (MNT) into the cancer patient journey by leveraging current existing technology?
Sub-Questions
- What is the current pathway for MNT services (hospital vs. outpatient)?
- What barriers and facilitators do healthcare professionals encounter in educating the patient about the importance of nutrition?
- What barriers and facilitators do patients encounter when communicating their symptoms and needs to healthcare professionals?
- Why is cancer malnutrition overlooked or underdiagnosed during the treatment process?
Methodology
Action Research, also known as Participatory Action Research (PAR), is an approach commonly used to improve conditions and practices in various healthcare environments. The basic principle of action research is that one can learn through action through a wide variety of evaluative, investigative, and analytical research methods. This approach is useful for generating solutions to practical problems and empowering practitioners by getting them to engage with research and subsequent “development” or implementation activities.
Methods
The first phase of this research project was to understand the problem from multiple perspectives of the cancer care team and former patients. The primary data collection method was semi-structured interviews resulting in rich qualitative insights on the vital role of nutrition during the active treatment cycle and survivorship. The second phase required generating a potential solution with stakeholders to address the main challenges and barriers of Medical Nutritional Therapy (MNT) access. To identify touchpoint opportunities within the cancer-patient journey, I held a co-design workshop with each group to which every member contributed a unique idea or perspective towards solving the problem. The final phase (TBD) involves prototyping and testing to ensure the solution remains simple, intuitive, and grounded in patient values and desires. The group will also discuss and co-create standards and metrics of success to measure impact over time.
Qualitative Data Analysis
After running 20+ interviews with oncologists, former patients, dietitians, and nurses, I conducted QDA and highlighted and pulled quotes from each transcription that answered my main research questions or remained salient and insightful. Each selection then received a respective code to capture the phrase's main points or attributes. As codes began to aggregate, I reorganized each unit and sorted them into distinct categories, summarizing the entire unit's learnings. At the end of the organization process, I noted several patterns between groups. So I took the extra step of performing a cross-analysis, grouping similar categories to form a major theme.

Final Output
Some major themes include the following:
Different referral processes (influenced by lack of time and HCP awareness of resources): "The reality is with clinicians, it (nutrition) is just not on their minds. Their mind is busy and an hour behind all time and clinics. The first words out of my mouth with every single patient is, "I'm sorry I'm running behind."
Patients experiencing appointment overhead: "I also feel that sometimes the patients, especially in the active treatment setting, can be so overwhelmed with everything else, and I place the referral but do they actually keep the appointment for it?"
MNT intervention and nutrition as a source of empowerment: "Nutrition is the one positive in treatment plans. It's something that these people can do. It's something that's within our control. It's something that empowers them."
Providing evidence-based nutritional resources (avoiding misinformation): "Everyone thinks they're an expert at nutrition out here and now with one hour, just general guidelines, they want to do it on their own."
The final output consists of a high-level diagram visualizing how each major theme informs or influences the other. Additionally, I’ve highlighted pain points (red outline) and opportunities (green fill). Neutral aspects are highlighted in blue.

Co-Design Workshop
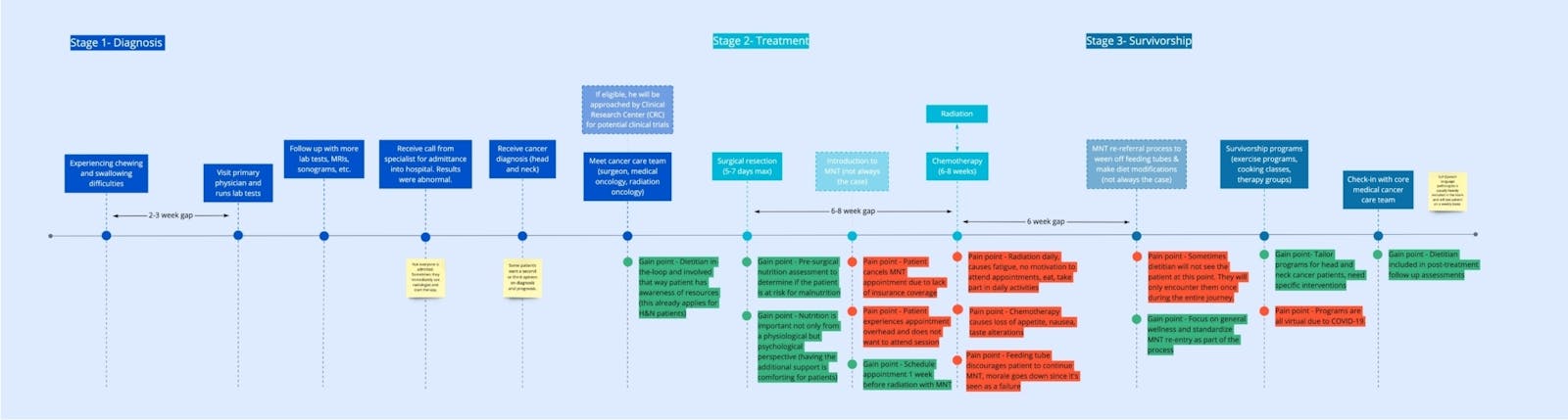
The co-design workshop took place virtually online with dietitians, patients, one oncologist, and one medical researcher. The group mapped out the patient journey for a typical head & neck cancer patient with the goal of identifying gain and pain points at specific touch points. We also ideated several potential solutions based on the highlighted opportunities.
Potential Solutions (TBD)
This phase of the research project still remains in- progress. Some ideas proposed by the group members of the co-design workshop are listed as follows:
Virtual calendar or patient diary - Documents journey and recommends appointments "Have you had this appointment yet?" including MNT and palliative care services.
A program that automatically refers patients at-risk of cancer malnutrition - Potential features and indicators: SMART SET in EPIC. % weight loss, indicated patient interest, lab abnormalities. *This idea does not pertain to head and neck cancer patients since these patients always see a dietitian, but this would allow the team to capture more types of patients they wouldn't usually capture.
Set patient goals in the shared electronic platform (including nutritional goals) - This will help align the cancer care team and possibly allow for more collaboration between the medical and palliative care teams. Use PHQ-9 (or any standardized depression or anxiety scale) to monitor mental health. Integrate with Redcap to collect data and administer surveys digitally.
